Exercise Associated Hyponatremia (EAH)
So, you signed up to work the Leadville 100 as medical crew but there’s no serum sodium analysis on-site capability. Differentiating between dehydration and hyponatremia can be difficult. The bias tends towards dehydration when confronted with non-specific symptoms such as nausea, headache, lethargy, etc. when in this context. Recent studies, however, show that 67% of ultramarathon runners in one race had EAH,¹ and 13% in the 2020 Boston Marathon with 0.6% of those being critical.²
Plash, Walker MD FAWM, presented “Being in Balance in a Salty World” at the Wilderness Medical Society winter conference 2023 in a manner to help clarify focus on the more objective historical and measurable symptoms rather than the often vague and non-specific symptoms and signs classically presented in wilderness medicine education.
As in all of wilderness medicine, prevention is everything. The latest Wilderness Medical Society guidelines are to “drink to thirst” as in, subjective perception of thirst should indicate when to drink to prevent overhydration rather than prescribed amounts of fluid per hour. However, the perception of thirst can be altered by certain medications, or Syndrome of Inappropriate Anti-Diuretic Hormone (SIADH) may be at play. Psychotropics; SSRI’s, amphetamines, and anti-seizure/mood stabilizing medications can all be culprits (Other medications can too, but the populations utilizing them are perhaps less likely to be taking on the Leadville 100 or Grand Traverse backcountry ski tour).
Therefore, since the GI tract can only absorb approximately a liter of fluid per hour and the kidneys can only process a liter of fluid per hour, if a recommended guideline of intake needs to be given it is commonly accepted to be 400–800 ml (2–4 cups)³ per hour. Most “sport” fluid replacement drinks do not contain adequate sodium to prevent hyponatremia. Consider newer gels like Huma Electrolytes Plus or electrolyte replacement hydration with salt, like Scratch. The salt is easier for your body to obtain when mixed with fluid than as solid fuel (Dina Griffin; MS, RSN, The Nutrition Mechanic).
Diagnostically, focus on:
Mild EAH
• Fluid intake history; large (relative if SIADH exists)
• Weight gain or “bloated” feeling
• Vital signs; normal
• No orthostatic changes (no dizziness when standing)
Severe EAH
• Large fluid intake (generally 1.0–1.5 liters per hour or more)
• Shortness of breath at rest
Mild Dehydration
• Fluid intake; small
• Thirst is present
• Orthostatic changes (is dizzy with upright position)
• Dry mucous membranes
Heatstroke
• History of little fluid intake
• Confirmed or suspected Temp> 104 F
Random points: Lack of urine production does not always indicate dehydration instead of hyponatremia. Because of the potential existence of SIADH, people with hyponatremia do not always present with a high urine output as is often taught.
Altered mentation is present in both severe dehydration and hyponatremia and could cloud a differential diagnosis as well.
You can expect a spike in hyponatremia symptoms after a long race is over; due to the physiology of how the body absorbs fluid from the GI tract.⁴
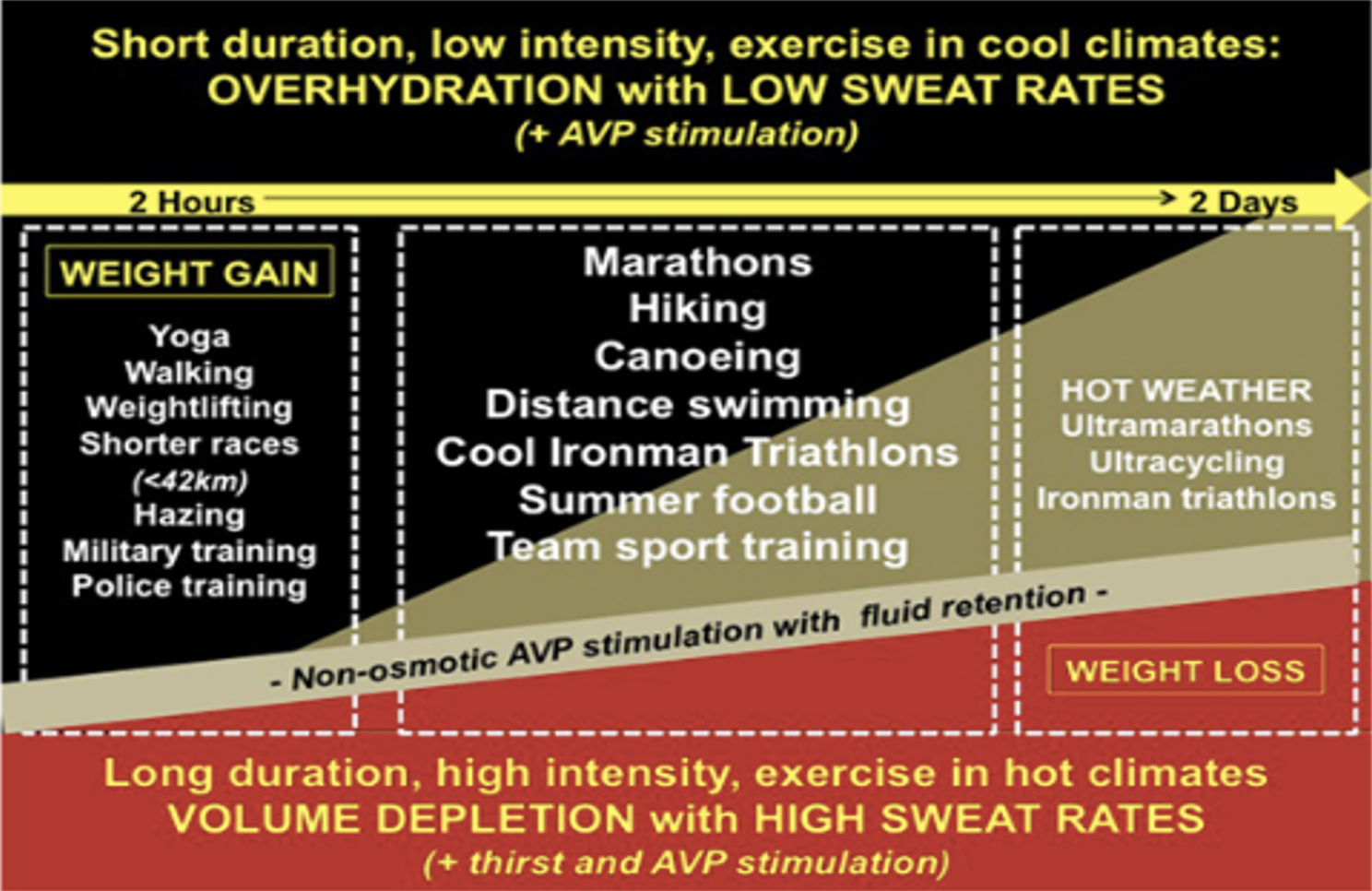
The chart below examines the contribution of overhydration w/arginine vasopressor (AVP) stimulation vs. high sweat rates/AVP stimulation even in the context of volume depletion. (In other words, there are many ways to conclude that perhaps you need to go a size larger in your lycra onesie team suit…
(AVP is the same as anti-diuretic hormone)
(Reprinted per open access fair use; “Exercise-Associated Hyponatremia; 2017 Update. Front. Med, Nephrology. 2017; 4:21.)
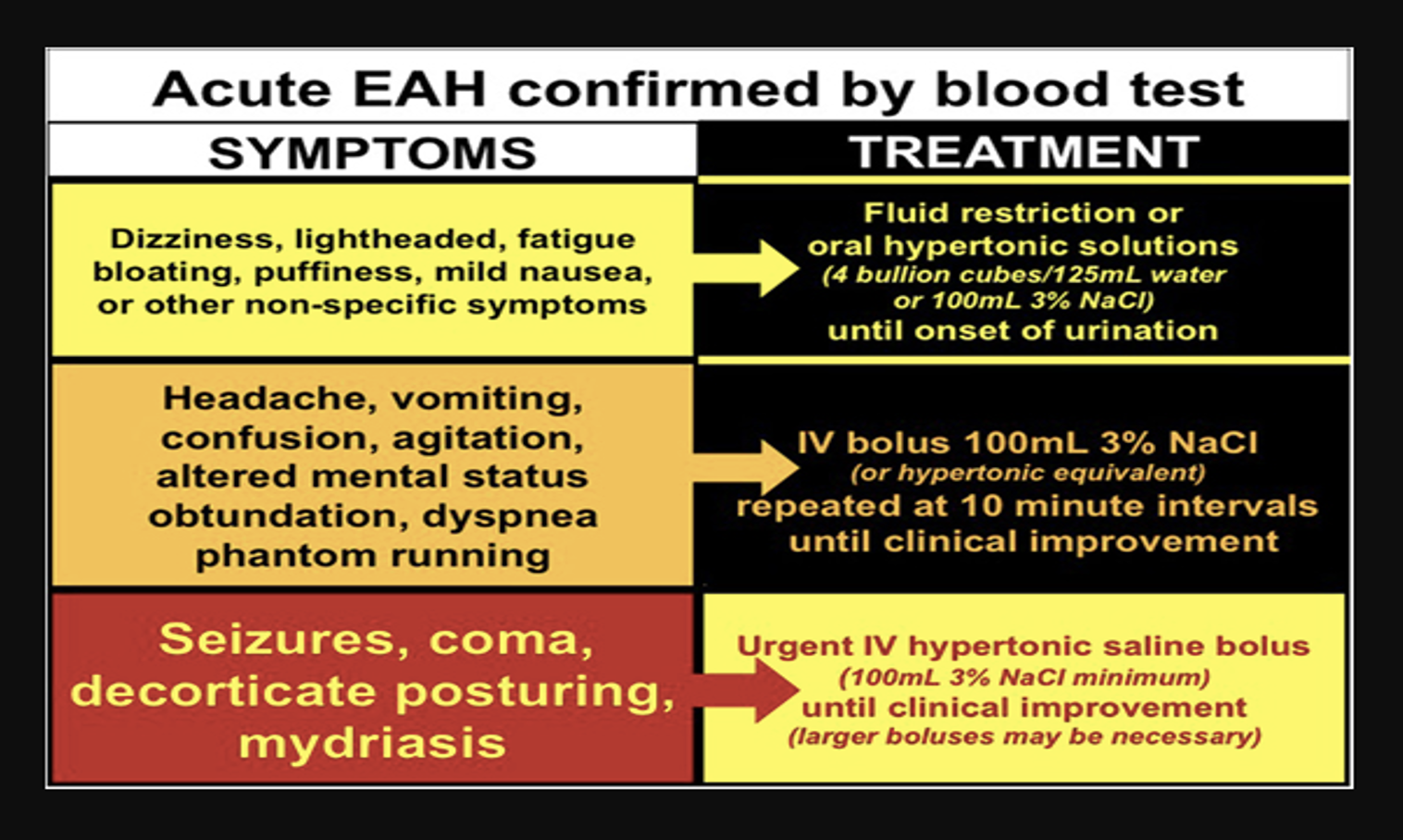
Treatment
Mild EAH
• Fluid restriction
• Oral Sodium
• Let’s talk about this: the WMS currently recommends 4 bouillon cubes in ¼ cup water. I tried it. It will cloud your differential diagnosis by the introduction of the non-specific but ever-present vomiting symptom in hyponatremia, but you get the idea…
• Avoid hypotonic and isotonic fluid, either IV or oral. Gatorade and other things like it are not hypertonic.
Severe EAH
• Evacuation
• Hypertonic fluid; 100ml of 3% Every 10 minutes (WMS guideline)
Dehydration
• 400–800 ml H20 or electrolyte mix/hour, small sips
• Normal saline IV fluid
Prevention
It is possible to take a simple test to find out how much sodium you should be taking during exertional activities. Out of interest prior to a couple of long mountain bike endeavors last summer, a riding partner and I took this test. The results were very enlightening and useful. He is a heavy sweater and was undertaking the 6–day EPIC mountain bike race at the time. His “sweat sodium concentration scale” (mg of salt produced per liter of sweat) was significant and rated “very high” at 1678 mg/L whereas I came in at “average” (no surprise…) at 819 gm/L. This ratio is genetically determined and unchangeable physiology, whereas fluid lost per endeavor can be influenced by heat, distance and intensity of exertion, fitness level, fluid status, and menstrual cycle.
The recommendation is to replace 65–90% of sodium loss in conditions of longer duration, high heat and/or high humidity. I came out with a recommendation to take in 350–450 mg sodium per hour; that’s way higher than usual intake for me, and, combined with the recommended pre-loading of fluid and sodium I felt way better than I ever have during a high output outing of long duration after implementing this guideline. For my friend, it was like a performance enhancing drug and he finished in the top 7% of the Grand Traverse in hot conditions shortly after the EPIC by addressing his extensive sodium needs.
So, think about adding a few potato chips to your handful of Skittles at that next aid station in a long race. And add a few bouillon cubes to your first aid kit on long outings; both winter and summer.
Kind regards,
kl
References:
Hew-Butler T, Loi V, Pani A et. al. Exercise – Associated Hyponatremia; 2017 Update. Front. Med, Nephrology. March 2017.
Almond CS MD, Shin AY MD, Fortescue EB MD, et al. Hyponatremia Among Runners in the Boston Marathon. N Engl J med 2005; 352.
Rosner M, Kinen J. Exercise Associated Hyponatremia. Clin J Am Soc Nephro. January 2007. 2 (1).
Hew-Butler T; EAH 2017 Update